This Week in Health: Restless Legs Syndrome
Restless Legs Syndrome Or why I have the "Jimmy Legs" Overview Restless legs syndrome (RLS)…
This Week in Health: Skin Cancer
End of Summer Time for Your Annual Mole Patrol Visit Three Main Types of Skin…
This Week in Health: Plantar Fasciitis
Plantar Fasciitis Or Why My Heel is Killing Me! Overview Plantar fasciitis is one of…
HEALTH: Computer Ergonomics
Ergonomic Tips for Computer Users How to Protect Yourself from Strain and Pain Overview Ergonomics…
This Week in Health: Oh My Aching Head
Migraine Headaches Less Despair and Greater Hope These Days Introduction Migraine management is a weighty…
Health: Hotter than Hell?
Heat Exhaustion & Heat Stroke Don't Let it Happen to You or Your Friends Overview…
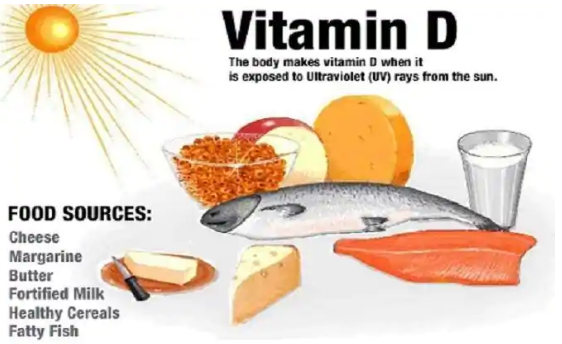
This Week in Health: Vitamin D deficiency
Vitamin D Deficiency More Common than You Would Think Overview Vitamin D isn't a single…
Health: What’s Bugging You?
What's Bugging You? Insect Borne Diseases Since it is summer, and many of us are…
This Week in Health: Insomnia
Insomnia - or why the hell can't I sleep? A Very Common Problem for Veterans…